Diagnosing a CASK gene disorder
Many females with MICPCH are first diagnosed with microcephaly and developmental delay thereafter receive an MRI to image the brain. A diagnosis of PCH (pontocerebellar hypoplasia) may be given to the families, who will await genetic results to confirm the genetic cause of the PCH.
In the UK it can take six months to receive the genetic test results to confirm a CASK mutation. Below we highlight the radiological features to help distinguish between some forms of PCH and CASK-related MICPCH, enabling families to get a more definitive answer faster. Any diagnosis should always be followed up by a genetic test to confirm a CASK mutation.
Distinguishing between CASK-related MICPCH and PCH type 2 and 4
Although CASK is the most frequently mutated gene associated with PCH, it is one of the least well-known and often over-looked.
The majority of female patients with a mutation in their CASK gene have an underdevelopment of the cerebellum, the cerebellar vermis, and the pons, called pontocerebellar hypoplasia (PCH). Usually, there is a proportionate involvement of the cerebellar vermis and hemispheres, contrary to what is found in PCH type 2 and type 4 (Moog et al. 2011). These types of PCH are predominantly associated with flat cerebellar hemispheres and small but less severely affected vermis, giving a dragonfly-like appearance to the cerebellum.
In female patients with a CASK mutation the corpus callosum tends to have a normal size. Since the corpus callosum is normal in size and the cerebrum is smaller in size (because of the microcephaly), this can give the impression of thickening of the corpus callosum (Takanashi 2010).
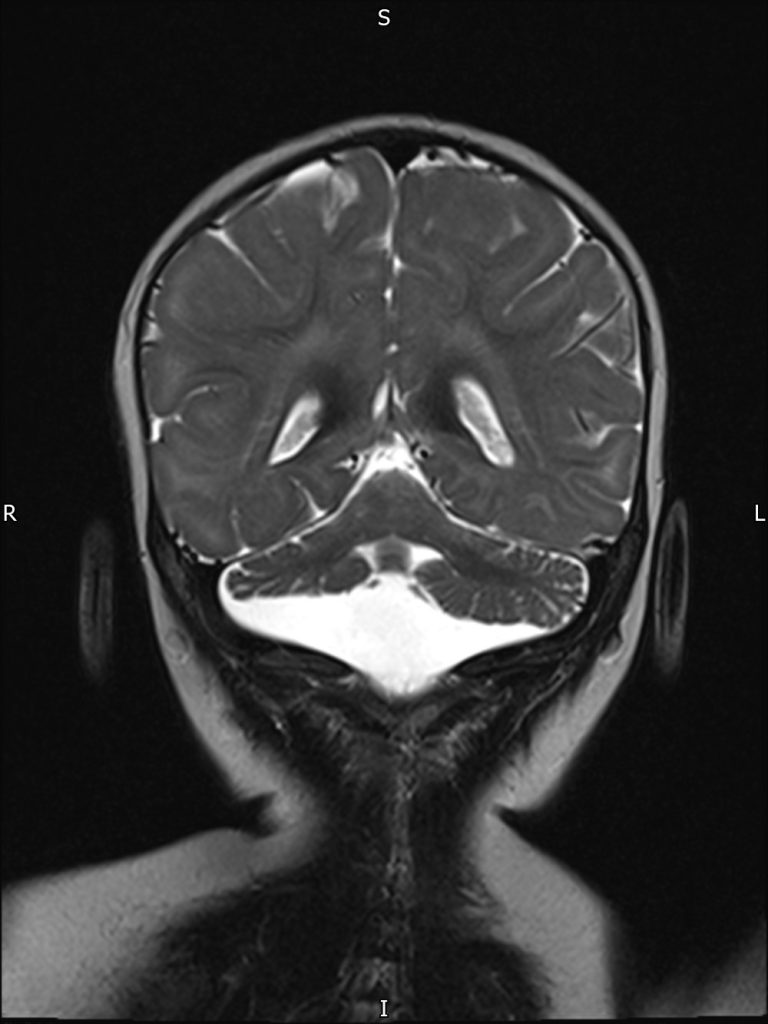
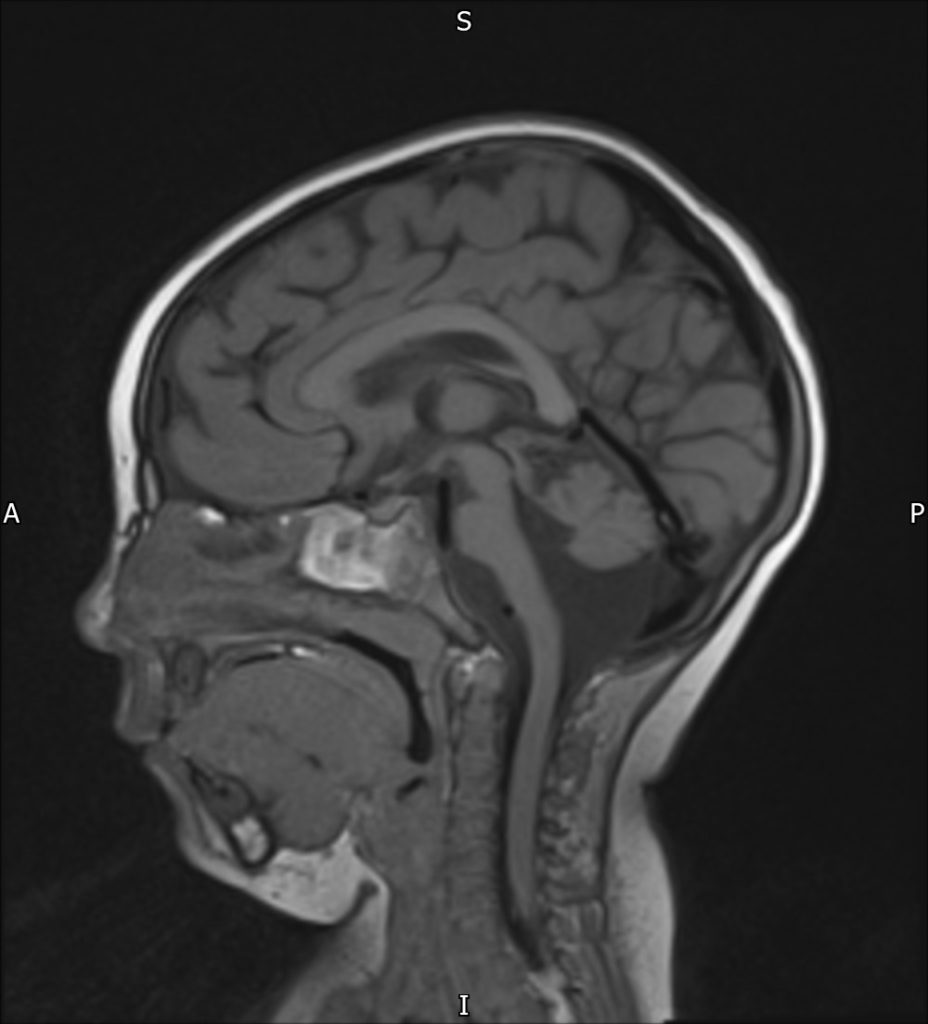
MRI images of a patient with a CASK mutation displaying typical MICPCH features.
In addition to brain imaging results, specific clinical features, or the absence of them, can assist in differentiating a CASK-related disorder from PCH type 2. Generalized clonus (“jitteriness”), lack of voluntary motor development, spasticity, impaired swallowing, and epilepsy shortly after birth are commonly associated with PCH2 but are rarer or absent in female patients with CASK mutations, whilst sensorineural hearing loss may be suggestive of CASK. See (https://pubmed.ncbi.nlm.nih.gov/20301773/) and https://www.ncbi.nlm.nih.gov/books/NBK169825/
We are grateful to Professor Kutsche and Dr Amin for assisting us with this summary.

